Dr. Edward Boshnick spearheads an advanced optometric practice dedicated to restoring vision and comfort lost due to a variety of eye conditions and surgeries, such as LASIK, keratoconus, and corneal trauma. His comprehensive services include non-surgical vision improvement, specialized contact and scleral lens care, pediatric vision, and vision rehabilitation for the partially sighted. Dr. Boshnick earned his B.A. degree from the University of Miami and was awarded his Doctorate in Optometry from Southern College of Optometry.
7800 SW 87 AVE SUITE B-270 MIAMI, FLORIDA 33173
305-271-8206
Contact Us

Welcome to Global Vision Rehabilitation Center
Dr. Boshnick's Expert Eye Care Services
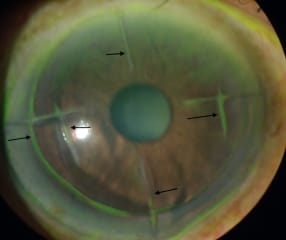



Corneal Dystrophy and Degeneration
Categories Lasik Complications All Laser Lasik Cornea & Glaucoma Eye ...
04



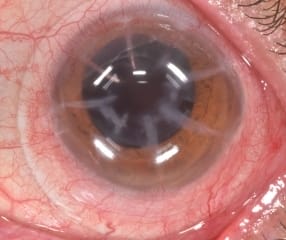
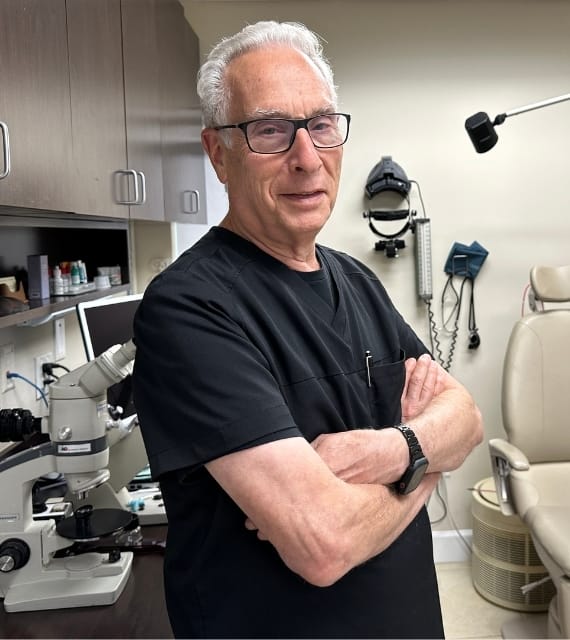
Radial Keratotomy Complications
Categories Lasik Complications All Laser Lasik Cornea & Glaucoma Eye ...
09
Experience and Expertise: Why Choose Dr. Boshnick
- Eye Treatment
- Contact Lenses
Choose Dr. Boshnick for personalized, comprehensive vision care backed by vast experience with complex eye conditions.

- Nsectetur cing elit
- Suspe ndisse suscipit sagittis leo
- Entum estibulum dignissim posuere
- Lorem Ipsum on the tend to repeat
Choose Dr. Boshnick for personalized, comprehensive vision care backed by vast experience with complex eye conditions.

- Comprehensive Eye Care: Provides full range of vision care services.
- Personalized Approach: Each patient is given individual attention.
- Experience: Over 30 years of expertise in the field.
- Specialized in Complex Cases: Expert in treating complicated eye conditions.
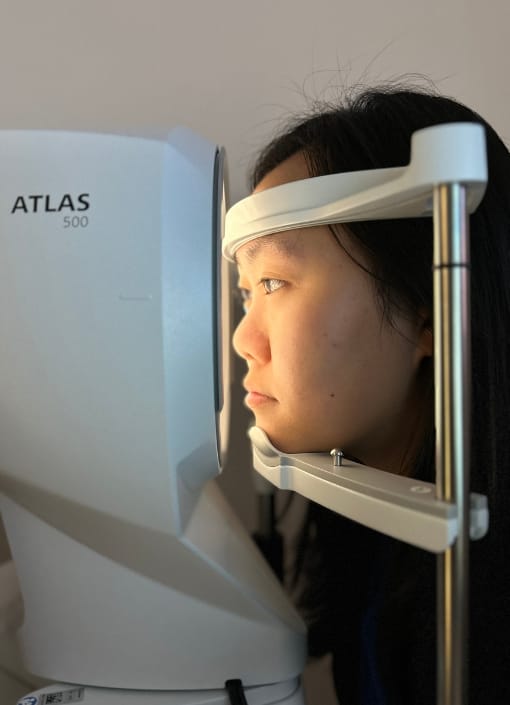
- Cutting-edge Technology: Uses the latest tech in optometric practice.
- Global Patient Base: Serves a diverse patient base from all around the world.
25,000+
Satisfied PatientsSchedule Your Consultation with
Dr. Boshnick
-
-
-
7800 Sw 87 Ave Suite B-270
Miami, Florida 33173
Dr. Boshnick's Modern Approach: Our Advanced Technologies
Dr. Edward Boshnick's practice leverages advanced technologies
Dr. Edward Boshnick's practice leverages advanced technologies to offer top-tier vision care. He uses state-of-the-art diagnostic equipment and cutting-edge treatment methods, ensuring accurate diagnoses and effective treatments. This, coupled with his expertise, allows him to manage complex eye conditions with precision. With a commitment to staying abreast of technological advancements in optometry, Dr. Boshnick continues to innovate in his approach to eye care, delivering excellent patient outcomes.
Have any questions?
Schedule a Consultation

Sharing the Vision: Testimonials for Dr. Boshnick
Dr. Boshnick has been my doctor for a few years now. If it weren’t for him and his expertise, I would be far worse and not receiving the treatment and care I need for my condition. From him to the students, to the wonderful ladies at the front desk, I am very grateful for him!
Dahila B
CustomerDr. Boshnick and his team have done such a great job when it comes to fitting me with contact lenses. They have listened to all of my concerns and didn’t stop until I was happy with the results. I haven’t seen this clearly in a long time!
Gage Boozan
CustomerUpon seeing Dr. Boshnick you are not just another patient, but you enter a long term relationship with him. He is very experienced and goes to great length to get you the best vision possible. He understands the emotional side that someone is going through with lasik complications and cares. We need more Doctors in this world like him.
Steven Jantzen
CustomerLatest Eye Care Insights: Latest From Our Blog

28 Jun
Scleral Lenses: An Innovative Solution to Chronic Dry Eye Syndrome
Scleral Lenses: The Ultimate Dry Eye Syndrome Solution Summary ...

25 Jun
Sculpting Sight: Exploring Scleral Lenses as a Solution to Keratoconus
Sculpting Sight: Exploring Scleral Lenses as a Solution to ...

24 Jun
Harnessing the Power of Scleral Lenses: A Revolution in Fuchs Corneal Dystrophy Treatment
Harnessing the Power of Scleral Lenses: A Revolution in ...

We only give best care
to your eyes.